The Hindu Editorial Analysis
24 May 2025
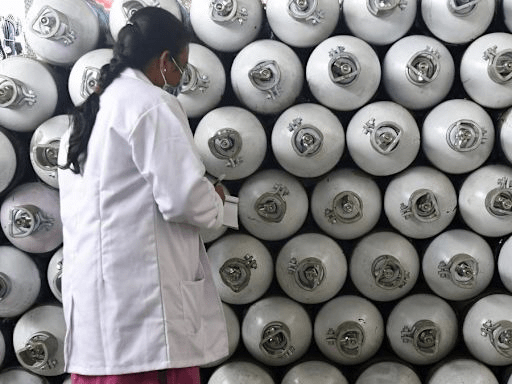
A medical oxygen access gap SE Asia must bridge
(Source – The Hindu, National Edition – Page No. – 08)
Topic: GS 2 & GS 3: Health Infrastructure | International Health Policy | Inclusive Development | SDG 3 (Good Health and Well-being)
Context
- South and Southeast Asia face the highest demand for medical oxygen, but access and infrastructure remain highly unequal, especially in low- and middle-income countries (LMICs).
- The editorial outlines why oxygen access is a life-saving but under-prioritised health equity issue, made more urgent by the COVID-19 experience.
Introduction
Oxygen saves lives, yet for millions, it is still out of reach.
Despite global acknowledgment of oxygen as a medical necessity, many LMICs in Southeast Asia face critical shortages in production, delivery, and affordability.
Bridging this gap isn’t just about healthcare—it’s about justice, preparedness, and human dignity.
The Access Crisis: Lessons from COVID-19
1. Infrastructure Deficiency and Equipment Gaps
- Only 54% of hospitals in LMICs have continuous oxygen supply.
- Most rely on outdated cylinders and concentrators with no local repair capacity.
2. Financial and Human Resource Shortfalls
- Governments struggle to sustain procurement and repair.
- Lack of trained biomedical engineers leads to frequent breakdowns.
3. Inequality in Distribution
- Remote and underserved communities suffer most, lacking stable access.
- Health providers in LMICs often face increased mortality risks due to diagnostic and treatment delays caused by oxygen shortages.
Why This Matters: Health, Equity, and Emergency Preparedness
1. Medical Oxygen Is an Essential Medicine
- WHO classifies oxygen as essential for treating pneumonia, sepsis, obstetric emergencies, trauma, and COVID-19.
- Without it, diagnostic and treatment chains collapse.
2. A Cross-Sectoral Responsibility
- Governments, donors, private sector, and civil society must collaborate to:
- Build robust supply chains
- Train technicians
- Create low-cost, resilient oxygen delivery models
What Needs to Be Done
1. A Coordinated Policy and Legal Framework
- Countries should align their oxygen strategies under a national roadmap that includes:
- Standardised protocols for transportation and storage
- Inclusion in universal health coverage
- Data-driven, transparent governance mechanisms
2. Infrastructure and Innovation
- Focus on Pressure Swing Adsorption (PSA) oxygen plants, now scaled in Bhutan, Nigeria, and India.
- Empower local production and repair ecosystems using scalable, solar-powered, or hybrid delivery systems.
3. Human Resource Capacity and Regional Collaboration
- WHO and national health training centers must scale up:
- Biomedical engineer training
- Cross-border partnerships for procurement, logistics, and maintenance
4. Real-Time Monitoring and Adaptability
- Use digital tools to manage supply chains, track failures, and forecast demand (e.g., using AI and predictive analytics).
Conclusion
- The oxygen crisis is solvable. What’s lacking is political will and investment priority.
As the Lancet Global Health Commission has urged, oxygen must be treated as a core part of health system equity, not a luxury. - Southeast Asia has the capacity, partnerships, and knowledge—what’s needed now is execution, funding, and sustained policy focus.
- Let us not wait for another pandemic to teach us what equity, preparedness, and health justice truly mean.


